by Jaime Tartar PhD – “If the glove don’t fit, you must acquit.” – Johnnie Cochran – Wacky Attorney
Why Do I Need to Write This? – If Johnnie Cochran was a scientist, he’d certainly acquit cortisol. But before I get ahead of myself, here’s a little background. Just so there’s no confusion, I’m not an expert in exercise science. The extent of my background here is that I jog regularly(ish) and lift weights often enough to psychologically validate my gym membership fees. I’m a Behavioral Neuroscientist which basically means that I like to know how the brain and body influence each other (it’s a good gig if you can get it especially in South Florida). Because much of my background and training has been focused on the neurobiology of stress, I find myself getting eye-twitchy and moaning inwardly quite often. It seems that there are some areas of science where anecdotal ideas and misinformation pervade and no one (in my humble, yet biased, opinion) has been more of a victim to this than my good buddy, cortisol. Facebook anyone?  This poor little bugger (aka cortisol) has gotten so beat up and kicked around that he could serve as the protagonist of a Victor Hugo novel. Understanding why cortisol is not “bad” is pretty straightforward. In order to help fix the tarnished reputation of cortisol I would like to consider and correct a few key ideas. Necessarily, this begins with a quick and painless overview of the network in which cortisol acts; actually there are some cool points here that can offer winning facts to pepper into a random conversation.
This poor little bugger (aka cortisol) has gotten so beat up and kicked around that he could serve as the protagonist of a Victor Hugo novel. Understanding why cortisol is not “bad” is pretty straightforward. In order to help fix the tarnished reputation of cortisol I would like to consider and correct a few key ideas. Necessarily, this begins with a quick and painless overview of the network in which cortisol acts; actually there are some cool points here that can offer winning facts to pepper into a random conversation.
SUPER QUICK Overview of Cortisol Release with Stress – So here we go; stress responses actually involve two major systems: the hypothalamic–pituitary–adrenal (HPA) axis and the sympathetic nervous system (SNS). The final product from the SNS in response to stress is 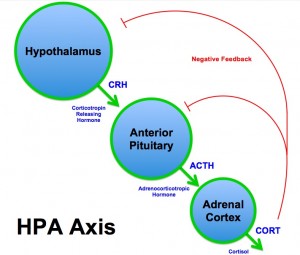 epinephrine (“adrenaline” if you’re nasty or European). This isn’t his story, though, so we are going to justifiably ignore him and just focus on the HPA system and cortisol for the current tale of woe and strife. While the response to stress through the HPA axis is intricate and complex, a review of the major players will suffice to shed light on why cortisol is an O.K. dude. The first step in the HPA stress response is that perceived or physical stress will induce the release of corticotrophin releasing hormone (CRH) from the hypothalamus in the brain. This guy then tells the pituitary gland to release pituitary adrenocorticotropic hormone (ACTH) into the bloodstream, who then stimulates the release of cortisol from the adrenal cortex (Hellhammer, Wust et al. 2009). The released cortisol does exactly what it is supposed to do to help deal with a stress. In response to stress, cortisol will mobilize energy for muscles, increase energy metabolism, increase cardiovascular tone, turn off nonessential activities, acutely increase immune function, and alter brain functions such as learning and perception processing (Aguilera 2011). However cortisol’s time in the limelight after stress is short-lived. It peaks about 30 minutes after the stressor and then further release is shut off through negative feedback regulation at all levels of the HPA axis and in an area of the brain called the hippocampus- he puts the breaks on the whole system at the level of the hypothalamus (from whence it all began). Cortisol levels are extremely tightly regulated and follow a predicable daily/circadian pattern of release (with the peak in the morning and the trough, or nadir, occurring at night). Although there is cortisol release with stress, the release is adaptive and helps to respond to increased energy demands – this is also why cortisol levels are high in the morning (known as the cortisol awakening response). This
epinephrine (“adrenaline” if you’re nasty or European). This isn’t his story, though, so we are going to justifiably ignore him and just focus on the HPA system and cortisol for the current tale of woe and strife. While the response to stress through the HPA axis is intricate and complex, a review of the major players will suffice to shed light on why cortisol is an O.K. dude. The first step in the HPA stress response is that perceived or physical stress will induce the release of corticotrophin releasing hormone (CRH) from the hypothalamus in the brain. This guy then tells the pituitary gland to release pituitary adrenocorticotropic hormone (ACTH) into the bloodstream, who then stimulates the release of cortisol from the adrenal cortex (Hellhammer, Wust et al. 2009). The released cortisol does exactly what it is supposed to do to help deal with a stress. In response to stress, cortisol will mobilize energy for muscles, increase energy metabolism, increase cardiovascular tone, turn off nonessential activities, acutely increase immune function, and alter brain functions such as learning and perception processing (Aguilera 2011). However cortisol’s time in the limelight after stress is short-lived. It peaks about 30 minutes after the stressor and then further release is shut off through negative feedback regulation at all levels of the HPA axis and in an area of the brain called the hippocampus- he puts the breaks on the whole system at the level of the hypothalamus (from whence it all began). Cortisol levels are extremely tightly regulated and follow a predicable daily/circadian pattern of release (with the peak in the morning and the trough, or nadir, occurring at night). Although there is cortisol release with stress, the release is adaptive and helps to respond to increased energy demands – this is also why cortisol levels are high in the morning (known as the cortisol awakening response). This 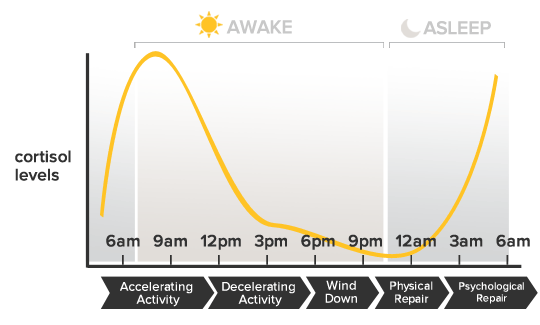 surge in a.m. cortisol helps to meet the energy demands needed to get moving and start a new day. In general, based on the negative feedback mechanisms that are in place for cortisol, we can rest assured that, in the absence of clinical disease or chronic stress (these ideas are reviewed at the end), cortisol is doing exactly what it needs to do to keep the body healthy and capable of dealing with a stress. Remember that cortisol reigns only briefly after stress and its actions here are beneficial in helping the body manage a perceived or physical challenge. Based on these ideas we can now clear up the three largest misconceptions of cortisol.
surge in a.m. cortisol helps to meet the energy demands needed to get moving and start a new day. In general, based on the negative feedback mechanisms that are in place for cortisol, we can rest assured that, in the absence of clinical disease or chronic stress (these ideas are reviewed at the end), cortisol is doing exactly what it needs to do to keep the body healthy and capable of dealing with a stress. Remember that cortisol reigns only briefly after stress and its actions here are beneficial in helping the body manage a perceived or physical challenge. Based on these ideas we can now clear up the three largest misconceptions of cortisol.
Cortisol is not a stress meter – Cortisol levels do not simply rise and fall as the body is stressed. This is subtle, and where some information is misconstrued, because, as reviewed above, cortisol will go up when the body is stressed; however, that is not the same thing as being a direct measure of stress. Cortisol levels do not correspond directly to the type and intensity of stress and there are many individual differences in cortisol release in response to stress. Also, cortisol levels do not go down in the absence of stress. Please re-read that phrase. We reviewed above a typical circadian cortisol pattern. This exists because ACTH is released continuously in pulses throughout the day; the pulses speed up or slow down because they are entrained to circadian processing in the hypothalamus (Veldhuis and Johnson 1991). Negative feedback regulation of the HPA axis ensures that cortisol levels don’t get too high for too long, and when they do, they are shut  down with rapid and decisive action. So we can appreciate that there is not signal for “Hey we are not stressed so let’s decrease cortisol!” That’s bonkers and makes no sense since cortisol is an essential hormone in the body. This leads to the second point.
down with rapid and decisive action. So we can appreciate that there is not signal for “Hey we are not stressed so let’s decrease cortisol!” That’s bonkers and makes no sense since cortisol is an essential hormone in the body. This leads to the second point.
Cortisol is not “bad for you” – it helps keep you alive! – Truly! Natural selection has ensured that in response to a stressor or challenge to homeostasis, cortisol does exactly what it is supposed to do. We all get to be alive today because our ancestors could mount an appropriate stress response. Furthermore, once cortisol is increased in response to stress or a change in homeostasis (e.g. through physical exertion), the changes are short-term. Chronically low cortisol levels can lead to decreased energy, muscle weakness, and low blood sugar. Critically, also, is that cortisol helps to reign in the immune system and helps prevent chronic inflammation and autoimmunity. For example, hyporesponsive HPA activity is seen in autoimmune disorders such as rheumatoid arthritis and chronic fatigue syndrome (Demitrack, Dale et al. 1991, Chikanza, Petrou et al. 1992)
Cortisol isn’t making you fat – Many people associate increased cortisol with weight gain. This viewpoint is prevalent in the fitness world. It’s true that elevated and sustained levels of cortisol levels can increase fat storage; especially in the abdomen and face. However, the key here is sustained elevations. For example we tend to see this body type in those with Cushing’s disease. These are individuals with pathologically high levels of cortisol. Weight gain with exercise is not likely to happen because of cortisol. This is a misconception probably partially 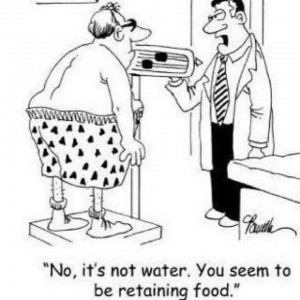 based off of misinterpretation of science. For example, one study demonstrated a correlation between cotrisol and weight gain (Epel, Moyer et al. 1999); this does not mean increased cortisol caused increased weight gain (this is why the mantra of every Introduction to Statistics class is “correlation does not imply causation”). Also, based on what we’ve reviewed about short-term cortisol actions, it would not make sense that cortisol “makes you fat” since the major role of cortisol during an intense exercise session is to mobilize energy resources to meet the immediate demands of the body. This primarily involves increased gluconeogenesis (converting glycogen to glucose), higher triglyceride levels, and increased blood flow to the heart and muscles (Majzoub 2006). Stress can cause weight gain; but this is through increased eating behavior not increased cortisol. Cortisol is an easy target, though, because pathologically or sustained levels of cortisol can cause increased fat storage. So the faulty thinking goes like this: exercise increases cortisol and cortisol causes weight gain. This is where that idiotic idea of too much cardio making you fat comes from. This is simply not accurate and a logical fallacy BUT it is an easy way to sell people a bunch of useless cortisol-fighting pills. Do you remember CortiSham? Ooops, I mean CortiSlim. The stuff worked about as well as giving a killer whale a bite of an apple and saying ‘hey Orca, I bet that filled you up.’ Increased eating that happens with chronic stress is complex and not directly due to cortisol levels. It is likely a product of individual differences in physiology, cognitive mechanisms, and a surplus of high calorie choices (Gibson 2006, Torres and Nowson 2007).
based off of misinterpretation of science. For example, one study demonstrated a correlation between cotrisol and weight gain (Epel, Moyer et al. 1999); this does not mean increased cortisol caused increased weight gain (this is why the mantra of every Introduction to Statistics class is “correlation does not imply causation”). Also, based on what we’ve reviewed about short-term cortisol actions, it would not make sense that cortisol “makes you fat” since the major role of cortisol during an intense exercise session is to mobilize energy resources to meet the immediate demands of the body. This primarily involves increased gluconeogenesis (converting glycogen to glucose), higher triglyceride levels, and increased blood flow to the heart and muscles (Majzoub 2006). Stress can cause weight gain; but this is through increased eating behavior not increased cortisol. Cortisol is an easy target, though, because pathologically or sustained levels of cortisol can cause increased fat storage. So the faulty thinking goes like this: exercise increases cortisol and cortisol causes weight gain. This is where that idiotic idea of too much cardio making you fat comes from. This is simply not accurate and a logical fallacy BUT it is an easy way to sell people a bunch of useless cortisol-fighting pills. Do you remember CortiSham? Ooops, I mean CortiSlim. The stuff worked about as well as giving a killer whale a bite of an apple and saying ‘hey Orca, I bet that filled you up.’ Increased eating that happens with chronic stress is complex and not directly due to cortisol levels. It is likely a product of individual differences in physiology, cognitive mechanisms, and a surplus of high calorie choices (Gibson 2006, Torres and Nowson 2007).
So what the hell cortisol – why the bad rep? – Most of the deleterious effects associated with cortisol come about as a result of chronic stress. While the HPA axis is well adapted to respond to threats, it is a reflexive physical response from the body and does not discriminate between real and perceived stress. A threat is a threat and it is was historically not adaptive for the brain to consider if something was really a threat before mounting a stress response. However, this can sometimes present problems to us “modern humans” since most of the things that stress us are not life threatening and are coming at us on a somewhat regular (chronic) basis. Humans living in industrialized nations are not likely starving, threatened by predators or, or battling for mating rights. Though if you went to a local pub you might wonder. However, we’re very good at experiencing chronic perceived emotional (sometimes imagined) chronic stress. In the absence of a disease process (e.g. Cushing’s disease) to cause hypercortisolemia, cortisol levels can become chronically  elevated when the HPA axis is dyregulated. While even amidst ongoing chronic stress (the daily life hassles we all experience), the HPA axis does a remarkable job of regulating cortisol. This is pretty amazing given that we do things like respond to an asshole in traffic the way we would a predator 10,000 years ago. And we got plenty of those in South Florida. Believe me. We might mount a stress response to assholes every day, while the predator only occurred once in a while. So, good on you HPA axis- you are doing a damn fine job! But (and this is where the mass hysteria arises) HPA axis dyregulation can come about from chronic stress through several ways. The big one here is unremitting and uncontrollable stress. So in order to really dysregulate the HPA axis, you really need to get in there and be sure that the stress is ongoing and that there is no habituation to the stress. In other words, if someone gets punched in the face regularly and predictably it stops becoming a stressor. So for those of you interested in “death by stress,” recognize that unpredictability and uncontrollability is essential to this. So pushing yourself in exercise won’t likely lead to a breakdown of the HPA axis since you have control and the act is predictable. To really do someone in, you might consider having that person run on a treadmill against his or her will and have the treadmill turn on and off at random times. Sounds like a CrossFit workout. LOL. Okay moving on. With that said, there are still some individuals that have an inability to adjust to regular, ongoing stress. These are what we call “high responders.” They mount a stress response very easily and seem to be in perpetual hypervigilance (I say “they” but I fall directly in this camp – knowledge is not always power?) There is evidence to suggest that these differences in stress sensitivity can be altered through stress in the womb (which changes the HPA axis “set point”) or through innate differences in physiological arousal- but this is an area that is greatly scientifically underexplored. Lastly, chronic stress can cause problems through rumination, or reactivation after stress has ended. If someone gets bitched out at work, that sucks, but since HPA activity is sensitive to psychological and physical insults, dwelling on the event and perpetually “reliving” it can cause a stress activation over and over, long after the actual event has passed. The problem with writing this is that I fear ruminators read it and ruminate on how they ruminate too much! So I suppose the take home message here is that chronic physical or psychological stress can produce chronically high levels of cortisol under very special circumstances. Exposure to chronic or severe stress (perceived or realized) can produce dysregulation of the HPA axis, which is characterized by enduring pathological hyper- or hyposecretion of cortisol.
elevated when the HPA axis is dyregulated. While even amidst ongoing chronic stress (the daily life hassles we all experience), the HPA axis does a remarkable job of regulating cortisol. This is pretty amazing given that we do things like respond to an asshole in traffic the way we would a predator 10,000 years ago. And we got plenty of those in South Florida. Believe me. We might mount a stress response to assholes every day, while the predator only occurred once in a while. So, good on you HPA axis- you are doing a damn fine job! But (and this is where the mass hysteria arises) HPA axis dyregulation can come about from chronic stress through several ways. The big one here is unremitting and uncontrollable stress. So in order to really dysregulate the HPA axis, you really need to get in there and be sure that the stress is ongoing and that there is no habituation to the stress. In other words, if someone gets punched in the face regularly and predictably it stops becoming a stressor. So for those of you interested in “death by stress,” recognize that unpredictability and uncontrollability is essential to this. So pushing yourself in exercise won’t likely lead to a breakdown of the HPA axis since you have control and the act is predictable. To really do someone in, you might consider having that person run on a treadmill against his or her will and have the treadmill turn on and off at random times. Sounds like a CrossFit workout. LOL. Okay moving on. With that said, there are still some individuals that have an inability to adjust to regular, ongoing stress. These are what we call “high responders.” They mount a stress response very easily and seem to be in perpetual hypervigilance (I say “they” but I fall directly in this camp – knowledge is not always power?) There is evidence to suggest that these differences in stress sensitivity can be altered through stress in the womb (which changes the HPA axis “set point”) or through innate differences in physiological arousal- but this is an area that is greatly scientifically underexplored. Lastly, chronic stress can cause problems through rumination, or reactivation after stress has ended. If someone gets bitched out at work, that sucks, but since HPA activity is sensitive to psychological and physical insults, dwelling on the event and perpetually “reliving” it can cause a stress activation over and over, long after the actual event has passed. The problem with writing this is that I fear ruminators read it and ruminate on how they ruminate too much! So I suppose the take home message here is that chronic physical or psychological stress can produce chronically high levels of cortisol under very special circumstances. Exposure to chronic or severe stress (perceived or realized) can produce dysregulation of the HPA axis, which is characterized by enduring pathological hyper- or hyposecretion of cortisol.
End on a positive! – Importantly for athletes, chronic stress in the form of endurance or exercise-induced increases in cortisol are not likely pathological or related to negative health consequences (Gerber, Brand et al. 2012). In fact, athletic training is associated with a decreased HPA response to an exercise challenge; it’s all about the habituation (Mastorakos, Pavlatou et al. 2005). Critically, also, is the overwhelming evidence that, despite HPA axis activation, regular exercise can also offer increased emotional well-being and protects against depression and other mood disorders (Galper, Trivedi et al. 2006, Lucas, Mekary et al. 2011, Hogan, Mata et al. 2013).
The bottom line is that exercise does increase cortisol, but these increases are not harmful and work to increase real energy demands on the body. Increased cortisol from exercise is not making anyone fat; that would be like blaming your fork for making you fat. Or chopsticks if you live in China. Instead blame increased eating with increased exercise. Go ahead and work out knowing, with great confidence, that cortisol is not your enemy. Donuts maybe, but not cortisol.
BIO – Jamie Tartar PhD earned her doctorate in the area of behavioral neuroscience from the University of Florida. She did her post-doctoral studies at Harvard Medical School’s Department of Psychiatry (2004-2006) and worked with the United States Army Reserves: Medical Service Corps (1998-2004). She is currently a professor at Nova Southeastern University in the  Department of Neuroscience. She loves brain stuff. One of her fellow Nova colleagues, Jose Antonio PhD, suggested this article topic because as he points out, there are too many self-appointed experts who think cortisol is the enemy. But as a smart dude once said: “Wisdom is a weapon, knowledge is the armour, and ignorance is the enemy.” Cortisol ain’t the enemy. Cotton candy maybe, ice cream perhaps, but cortisol? Nah.
Department of Neuroscience. She loves brain stuff. One of her fellow Nova colleagues, Jose Antonio PhD, suggested this article topic because as he points out, there are too many self-appointed experts who think cortisol is the enemy. But as a smart dude once said: “Wisdom is a weapon, knowledge is the armour, and ignorance is the enemy.” Cortisol ain’t the enemy. Cotton candy maybe, ice cream perhaps, but cortisol? Nah.
Science References For All You Nerds
Aguilera, G. (2011). “HPA axis responsiveness to stress: implications for healthy aging.” Exp Gerontol 46(2-3): 90-95.
Chikanza, I. C., P. Petrou, G. Kingsley, G. Chrousos and G. S. Panayi (1992). “Defective hypothalamic response to immune and inflammatory stimuli in patients with rheumatoid arthritis.” Arthritis & Rheumatism 35(11): 1281-1288.
Demitrack, M. A., J. K. Dale, S. E. Straus, L. Laue, S. J. Listwak, M. J. Kruesi, G. P. Chrousos and P. W. Gold (1991). “Evidence for impaired activation of the hypothalamic-pituitary-adrenal axis in patients with chronic fatigue syndrome.” The Journal of Clinical Endocrinology & Metabolism 73(6): 1224-1234.
Epel, E. E., A. E. Moyer, C. D. Martin, S. Macary, N. Cummings, J. Rodin and M. Rebuffe‐Scrive (1999). “Stress‐Induced Cortisol, Mood, and Fat Distribution in Men.” Obesity Research 7(1): 9-15.
Galper, D. I., M. H. Trivedi, C. E. Barlow, A. L. Dunn and J. B. Kampert (2006). “Inverse association between physical inactivity and mental health in men and women.” Medicine and Science in Sports and Exercise 38(1): 173.
Gerber, M., S. Brand, M. Lindwall, C. Elliot, N. Kalak, C. Herrmann, U. Pühse and I. H. Jonsdottir (2012). “Concerns regarding hair cortisol as a biomarker of chronic stress in exercise and sport science.” Journal of sports science & medicine 11(4): 571.
Gibson, E. L. (2006). “Emotional influences on food choice: sensory, physiological and psychological pathways.” Physiology & behavior 89(1): 53-61.
Hellhammer, D. H., S. Wust and B. M. Kudielka (2009). “Salivary cortisol as a biomarker in stress research.” Psychoneuroendocrinology 34(2): 163-171.
Hogan, C. L., J. Mata and L. L. Carstensen (2013). “Exercise holds immediate benefits for affect and cognition in younger and older adults.” Psychology and aging 28(2): 587.
Lucas, M., R. Mekary, A. Pan, F. Mirzaei, É. J. O’Reilly, W. C. Willett, K. Koenen, O. I. Okereke and A. Ascherio (2011). “Relation between clinical depression risk and physical activity and time spent watching television in older women: a 10-year prospective follow-up study.” American journal of epidemiology 174(9): 1017-1027.
Majzoub, J. A. (2006). “Corticotropin-releasing hormone physiology.” European Journal of Endocrinology 155(suppl 1): S71-S76.
Mastorakos, G., M. Pavlatou, E. Diamanti-Kandarakis and G. P. Chrousos (2005). “Exercise and the stress system.” Hormones (Athens) 4(2): 73-89.
Torres, S. J. and C. A. Nowson (2007). “Relationship between stress, eating behavior, and obesity.” Nutrition 23(11): 887-894.
Veldhuis, J. D. and M. L. Johnson (1991). “Deconvolution analysis of hormone data.” Methods in enzymology 210: 539-575.